When somebody's worst day unfolds, your support means our highly skilled crews can get to the emergency fast. For our doctors and paramedics, it’s a unique and rewarding part to play in the community. In this interview, Dr Neil Berry shares some insights behind the scenes of his role as an air ambulance doctor.
Have you always wanted to be an air ambulance doctor? Tell us how you got into this career.
I never planned to be an air ambulance doctor. When I first started out in medicine, I had my sights set on orthopaedic surgery. I didn’t know much about air ambulance work back then but, as time went on, I gathered experience in A&E departments and anaesthetics. That’s where I developed a real interest in trauma care. Then, when the chance came up to try something completely different for a year, I spotted a role with the Helicopter Emergency Medical Service at the Royal London Hospital.
That opportunity changed everything – and I haven’t looked back since.
How much training do you have to do before becoming an East Anglian Air Ambulance doctor?
East Anglian Air Ambulance initially employed me via the Royal London. My own training in the capital was intense, packed with lectures, simulations and hands-on learning – it was one of the most valuable experiences of my career. When I joined East Anglian Air Ambulance in 2012, I’d already been a doctor for 11 years, with five years of medical school behind me too.
Since I joined East Anglian Air Ambulance, I’ve been on around 1,500 taskings. It’s a privilege to be there for people when they need help the most, and to be part of a team that delivers such extraordinary care, right at the scene.
What does a typical shift look like for you?
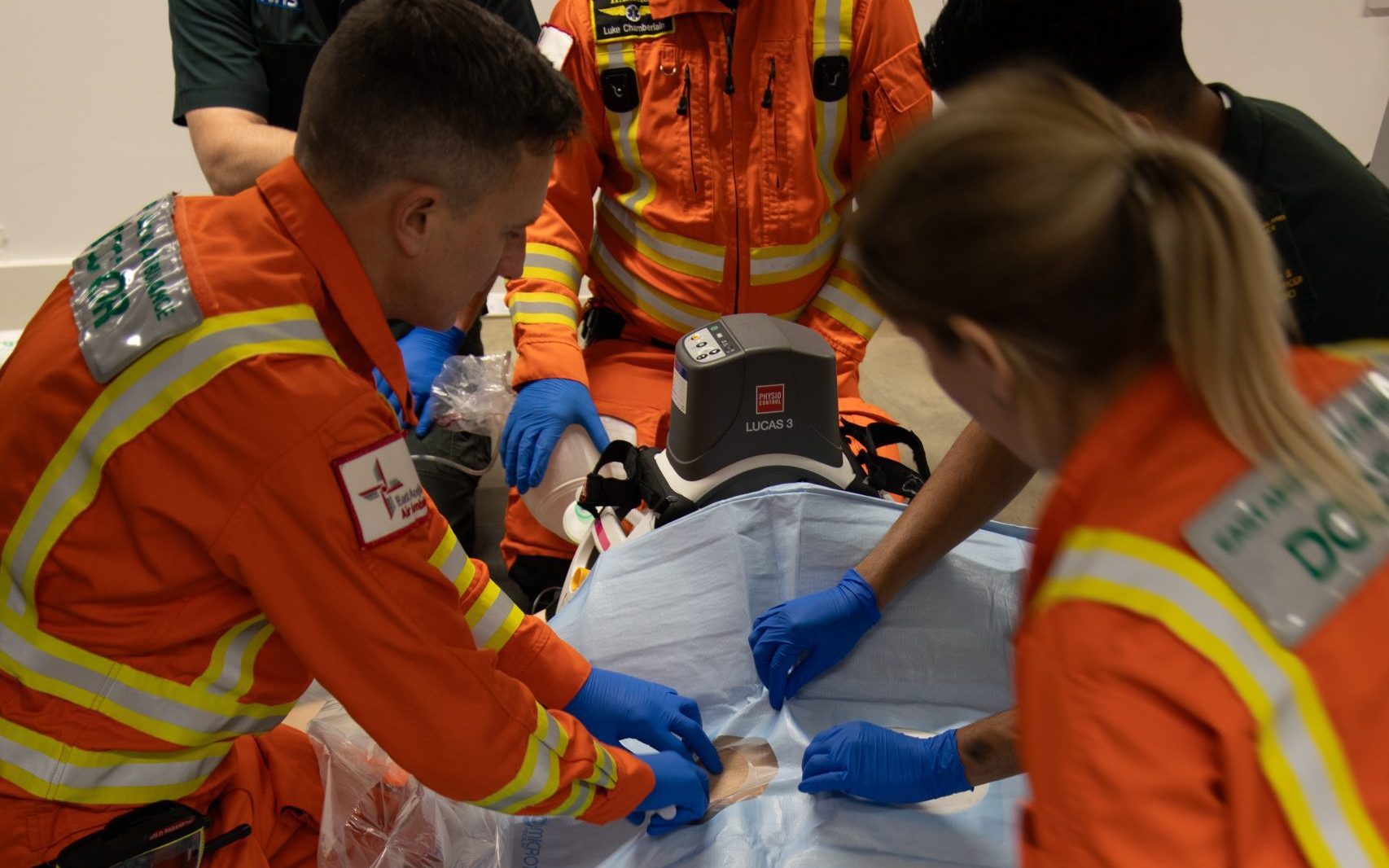
The Helicopter Emergency Medical Service is a unique world. At East Anglian Air Ambulance, we bring hospital-level critical care, by air and road, to people facing the worst moments of their lives. We operate 24/7 every single day of the year. Our team is made up of incredibly skilled doctors and critical care paramedics, each bringing their own experience and expertise to the job. That diversity is one of our greatest strengths.
Our shifts are 12 hours, either 7am to 7pm, or the other way around. I am usually based at Cambridge as part of the Anglia Two crew, although I do carry out shifts with Anglia One in Norwich too. I usually get to base about half an hour early to settle in. The first hour is full-on: checking kit and equipment, running through medication, and making sure the helicopter and critical care car are fully operational and good to go. We also have a briefing with the pilots, where they update us on weather conditions and anything else we need to know for the shift ahead.
After that, it’s a case of waiting for the phone to ring with a call-out. While we wait, we keep busy with training. Often, I’ll be working alongside a doctor or critical care paramedic who’s new to the charity, helping them get up to speed. But the moment that phone rings, we are ready to respond.
How many calls do you get a week/month?
Between our two bases in Norwich and Cambridge, we’re called out around eight times a day to help people in the worst moments of their lives. That could be someone in cardiac arrest to a person badly hurt in a road accident, or traumatic injuries in an equestrian incident.
Why might someone need an air ambulance over a normal ambulance? And what services can you offer patients in need?
A lot of people think calling 999 gets you the same response every time, but that’s not the case. We’re a vital partner of, and we’re proud to work alongside, the East of England Ambulance Service, Police and Fire and Rescue Service. We bring an extra level of care that can make all the difference. Our team can carry out critical interventions like surgery, anaesthesia, and advanced cardiac arrest management right there at the scene – before the patient even reaches the doors of A&E. When time matters most, we bring the hospital to them.
This, combined with quick onward transfer to the most appropriate hospital, gives every patient the best possible chance of surviving and recovering a life-threatening emergency.
How long does it take to respond to a call? And what’s going through your mind?
We work closely with the ambulance service to support them in identifying patients who may benefit from the advanced skills, equipment and medication our crew can bring to scene, at the earliest opportunity. Working in collaboration means patients can receive the best possible treatment and care during some of the worst moments of their lives.
We aim to be in the air or on the road within 3-4 minutes. We fly 24/7 from our Norwich base – the planning process for night flying takes a little longer as more detail is needed about potential landing areas are considered. There are many more safety considerations when it comes to night-time flying.
What’s the most memorable call you’ve ever been part of?
There are so many memorable tasks and memorable people – I never fail to be moved by the resilience of our patients and their families.
A particularly memorable incident was when we were tasked to help an injured kite surfer. A strong gust of wind had caught him and flown him into a sea wall. He had many injuries, including broken bones and internal injuries. He was critically unwell. Among the treatment we provided at the scene was a pre-hospital emergency anaesthetic so we could treat and stabilise him before flying to Addenbrooke’s Hospital.
The gentleman made a full recovery, and a few years later he gave a speech to the guests at a fundraising ball, which my wife had organised in aid of East Anglian Air Ambulance. It was a very poignant moment.
Do you ever meet patients again after you’ve treated them? If so, any that stand out?
We have a dedicated aftercare service for our former patients and families to help them navigate the often-challenging path following a life-threatening medical emergency. They offer practical and emotional support and, as part of this, they can facilitate meetings with the crew. I’ve attended many of these meetings and words can’t adequately describe how it feels to see our former patients months later. We are called to people and families in some of their darkest moments, so to see those who have had a positive outcome, and are on a path to recovery, however that may look for them, is truly special – it’s testament to our supporters and donors who make moments like this possible.
What makes the job rewarding enough to keep doing it despite the stress?
Working with such a great team, with wonderful camaraderie and support, alongside the vital work we carry out, is the most rewarding part of the job. We’re not just a yellow helicopter; we bring emergency care directly to where it’s needed in time-critical, life-threatening situations. Our work is innovative, cutting edge and so interesting. I feel extremely privileged to help people in their darkest moments – in many different environments, their homes, in town centres, in the countryside, often in austere environments and rapidly evolving situations. But knowing that we can make a difference to people’s lives – and we’re trusted to do so by our supporters and communities – is hugely rewarding and humbling.